News

Two television programs highlighting the experiences of people with disabilities seeking out romantic relationships are taking home some of television’s top honors. The Netflix show “Love on the Spectrum,” which chronicles the dating lives of adults with autism, won two Emmys, one for outstanding unstructured reality program and another for casting. Meanwhile, the documentary “Patrice: The Movie” won for exceptional merit in documentary filmmaking. The film, which aired on Hulu last year, follows Patrice Jetter who wants to marry her partner, but can’t because they both have disabilities and doing so could compromise their Social Security and Medicaid benefits. The awards were presented over the weekend at the Creative Arts Emmy Awards in Los Angeles where several honors were handed out ahead of the main Emmy Awards, which will be this Sunday. Presenters at the specialty Emmys included two cast members from “Love on the Spectrum,” Marlee Matlin, an actress who is deaf, as well as Nyle DiMarco, who is also deaf and is a director and producer of the AppleTV+ documentary “Deaf President Now!” “Love on the Spectrum” previously won five Emmys. The documentary series, which follows adults with autism from across the U.S. as they pursue dating and relationships, is a spinoff of an Australian version. Netflix has already renewed the show for a fourth season. “From the beginning, our aim has been to create a series that treats our participants with dignity and respect while offering genuine insight into their experiences,” said Cian O’Clery, director, executive producer and co-creator of the series. “These awards celebrate not only our production team’s efforts but also the courage of our participants who have touched millions with their personal journeys and helped reshape the public’s understanding of autism.” An edited broadcast of the Creative Arts Emmy Awards will air Saturday at 8 p.m. PT on FXX and will be available to stream on Hulu through Oct. 7. Citations : [ORIGINAL ARTICLE] https://www.disabilityscoop.com/2025/09/09/disability-focused-shows-win-emmys/31615/

One 17-year-old from Maryland has found a special way to honor her little sister with Down syndrome: by writing a book about her. Key Takeaways: Maryland high schooler Ava Perlin has written a book about her sister, Millie, called “One in a Millieon” as a way to foster inclusivity for those who have Down syndrome. Ava hopes the book will inspire others to see past the differences of those with special needs. The Details: Ava Perlin told WBALTV that her book, “One in a Millieon,” began as a school project to foster inclusivity for others — in particular, her sister Millie, who is three years younger than she. Perlin said she noticed that many kids in school were unsure how to treat Millie because she has Down syndrome. “The biggest thing I noticed with her in school was less of the stereotypical bullying and more distance,” she said. “People feared the unknown and didn’t know how to interact with people who were different.” When her 11th grade English teacher told the students they had to pick a passion project, Ava had the idea to create a book meant to foster inclusivity. “That word — inclusivity — has real meaning and value in our home,” Ava’s mom, Lauren Perlin, told the news outlet. “So, to think that Ava chose to write a story about this — the impact Millie had on her, and what inclusivity means to her — is special and powerful.” Ava’s school project garnered such a positive response that she decided to turn it into a published book, which is now available on outlets like Amazon, where it’s currently the number one new release in the Teaching Students with Developmental & Intellectual Disabilities category. One Amazon reviewer notes that the book is “A heartfelt message about the power of love, family, inclusion, acceptance and celebrating our differences.” The Bottom Line As people with Down syndrome are so often overlooked [...] the message of inclusion and acceptance cannot be overstated. As Ava told WBAL-TV, she hopes the book inspires people to be more open to those who are different. “I want them to be a little less worried about people who are different, and a little bit more comfortable being themselves,” she said. “These people just want to be themselves as well.”

President Donald Trump wants to cut $163 billion in federal spending next year, potentially zeroing out key disability programs, some of which are already pausing services because they’re running out of money. The White House unveiled a budget summary late last week known as a “skinny budget” that calls on Congress to slash funding for non-defense discretionary spending by 22.6% for the fiscal year starting in October. This would affect programs that Congress reauthorizes annually, but does not include mandatory programs like Medicare, Medicaid and Social Security. The summary offers little detail about how many disability programs would be impacted. However, a widely circulated budget document leaked last month from the U.S. Department of Health and Human Services offers clues. That document shows that the Trump administration wants to eliminate funding for protection and advocacy agencies, state councils on developmental disabilities, the lifespan respite program and university centers on developmental disabilities, among other programs, advocates say. The targeted disability programs are housed within the Administration for Community Living, which HHS said in March that it plans to break up. Jill Jacobs, executive director of the National Association of Councils on Developmental Disabilities, said she had hoped that Trump’s skinny budget would allay concerns about the leaked HHS budget, but she indicated that it ended up doing “just the opposite.” “It shows absolutely nothing about any Administration for Community Living (ACL) funding at all. Other operating divisions within HHS are identified, but there is nothing about disability, nothing about aging, nothing at all under the HHS category,” Jacobs said. “This makes things even more confusing — and worrisome.” Already many developmental disability programs are being squeezed because HHS has delayed distributing funding that was authorized by Congress in March. In recent weeks, Disability Rights New Jersey, Disability Rights Mississippi and Disability Rights Arkansas have announced that they would halt certain services — either temporarily or indefinitely — because they are running out of money. The groups are all federally mandated protection and advocacy organizations, or P&As, which exist in each state to provide free legal and advocacy services to individuals with disabilities. The organizations help students with disabilities access school services, investigate abuse and neglect in both private and state-run facilities for those with developmental disabilities and much more. “Our agency has been serving individuals with disabilities since the early 1980s, and this is the first time that we have had to cease taking new cases agency-wide. Congress has already approved (and) allotted these monies for our agency — we just are waiting to receive it,” said Polly Tribble, executive director of Disability Rights Mississippi. “Our federal mandate is to protect and advocate for vulnerable people in Mississippi and to root out abuse, neglect, and exploitation, but without our promised funding, if someone calls tomorrow and needs assistance, we can only refer them to another agency.” Tribble noted that the other agencies they refer to are also dealing with cuts and delays in federal funding. “If this crisis is not resolved immediately, we are facing devastating layoffs that will severely compromise our ability to protect and serve the disability community,” Tribble said. These organizations are not likely to be the last ones curtailing services, said Eric Buehlmann, deputy executive director for public policy at the National Disability Rights Network, an umbrella organization for P&As across the country. “Ultimately all P&As will be effected because they will run out funding to pay for staff and services,” he said. Representatives from HHS did not initially respond to questions about the payment delays, but the agency said on Monday that more than $1.1 billion in funding that Congress approved in March will be released by the Administration for Community Living in the next two weeks. The president’s skinny budget spells out cuts at the Centers for Medicare and Medicaid Services, the Centers for Disease Control and Prevention and the National Institutes of Health, among others. It seeks to consolidate housing assistance for people with disabilities with other programs and cut their funding. Spending on special education services would remain level, per the plan. But, seven programs under the Individuals with Disabilities Education Act would be consolidated to give “states and school districts greater flexibility” and funding for the Department of Education’s Office for Civil Rights would be chopped by 35%. “Level funding IDEA in particular — as proposed by the White House — is actually a cut,” said Denise S. Marshall, CEO of the Council of Parent Attorneys and Advocates, or COPAA, a nonprofit that advocates for the rights of students with disabilities and their families. That’s because funding has been static since 2023 even as the number of students with disabilities has grown, she said. The focus on cuts has advocates alarmed and programs operating in survival mode. “All of the uncertainty around funding has meant that disability programs are having to spend precious time and resources on contingency planning instead of focusing on supporting people with disabilities and their families,” said Alison Barkoff, a professor at George Washington University who led the Administration for Community Living under the Biden administration. “Programs that are critical to people with disabilities and their families are at serious risk now and heading into the next fiscal year,” she said, emphasizing that “the risk has never been more serious.” CITATION: [ORIGINAL ARTICLE] Nation’s Disability Services System Begins To Buckle As Funding Threats Intensify: https://tinyurl.com/8c7yx375

The moment that 20-year-old Eric Carpenter-Grantham of Silver Spring had prayed for finally came to Annapolis this year, when both chambers of the Maryland General Assembly passed the bill that he and his mother had championed. “ Eric’s ID Law ” will allow Maryland residents with “non-apparent disabilities” to opt in to a program that will place a butterfly emblem on their state ID or driver’s license. That symbol isn’t just a decorative flourish. It will indicate to anyone looking at it that the holder of that license or ID has a disability that isn’t immediately obvious. That could include deafness, autism, developmental disabilities or a mental health issue. Linda Carpenter-Grantham, Eric’s mother, explained the idea for the butterfly license came after the two had a hard conversation after the death of George Floyd at the hands of Minneapolis police in 2020. Eric has autism, and his mom explained to WTOP that as the mother of a young Black man with a disability, Floyd’s death left her worried. After their conversation, she explained that Eric, a teenager at the time, “was in tears, he was crying, and he said ‘Mom, we’ve got to do something.'” Eric told his mother that he had an idea: “I would like to make something to go onto the ID so that the police will know that me and my friends have autism so that they won’t hurt us if we ever get stopped,'” Linda said. Eric, who has plans to become a pastor, said he “was praying to God” to send him the right symbol to use. “We were thinking about different things like a star,” he said. But then the butterfly magnets they had on their refrigerator at home came to mind. “So I said, ‘Let’s do a butterfly. The butterfly represents hope, peace, freedom and change,'” he said, and that became the centerpiece of their campaign. “We just want to thank every single person who supported this bill from Day One!” Eric said. His future plans include going to college to get a degree in political science, and to eventually become a pastor. “We’re just waiting for the date when the governor will sign the bill, and we’re super excited to stand there and watch him sign it and receive the ink pen!” she said, referring to the custom of passing the pens used to sign bills into law to the people who worked to get the legislation passed. Citations: [ORIGINAL ARTICLE] Maryland drivers with ‘hidden disabilities’ could get butterflies on their licenses: https://tinyurl.com/54upd5tw

A documentary about the decades-long fight for disability rights culminating in the passage of the Americans with Disabilities Act is set to premiere. The film “Change, Not Charity: The Americans with Disabilities Act” follows the twists and turns of a grassroots movement that pushed Congress to mandate curb cuts, ramps and much more to allow people with disabilities access to American life. Relying on archival footage and interviews with activists, lawmakers and other key players, the one-hour film chronicles how the disability rights movement organized and took to the streets to lobby for the ADA in the face of strong opposition. Things came to a head with the “Capitol Crawl,” when people with disabilities including many wheelchair users dragged themselves up the steps of the U.S. Capitol, leading to the 1990 signing of the ADA. “I think the message of this film is that civil rights for people with disabilities are just as important as the rights that everyone either has or should have in our society,” said the film’s director, Jim LeBrecht, who has a disability and who is known for his work on “Crip Camp,” an Oscar-nominated documentary [01] about the origins of the disability rights movement. “There was a coming together of many people, disabled and non-disabled people. Legislators from both sides of the aisle came together in a bipartisan fashion,” he said, referring to the ADA. “I hope that our film will remind our viewers and those in power, that preserving the civil and human rights of people with disabilities benefits everyone.” Narrated by actor Peter Dinklage, “Change, Not Charity: The Americans with Disabilities Act” will air on PBS March 25 at 9 p.m. ET on “American Experience.” Citations: IMDB Webpage for Crip Camp: https://www.imdb.com/title/tt8923484 Original Article: [ARTICLE] PBS To Spotlight Story Behind The ADA: https://www.disabilityscoop.com

BALTIMORE -- A proposed bill in Maryland would allow residents to disclose "nonapparent disabilities" on their driver's licenses or identification cards. Eric's ID Law, or HB707, [01] would require the Motor Vehicle Administration (MVA) to add a certain symbol to licenses, ID cards or moped permits indicating that the applicant has a nonapparent disability. The idea was proposed by a Maryland family during an appearance on ABC's "The View," The Baltimore Banner reported. [02] The Carpenter-Grantham family had the idea after the 2020 murder of George Floyd [03] which sparked protests across the nation. "I realized that I have an African American son with an invisible disability," mother Linda Carpenter-Grantham said during the TV appearance. The bill was introduced in the state Senate during the 2024 legislative session but missed a deadline in the House. The proposed bill would require the MVA to establish public outreach programs to educate the public about the new symbols or notations. The MVA would work with disability advocates to design the symbols. The MVA would be prohibited from sharing information about an applicant's disabilities. The bill would also prevent the MVA from asking an applicant to provide proof of their disability or reject an application because the listed disability does not match other documents associated with the applicant. Under the bill, the Maryland Police Training and Standards Commission and Department of State Police would have to immediately implement training for police interactions with those who have nonapparent disabilities noted on their IDs. The bill will be the subject of a hearing on Feb. 13 at 1 p.m. What is a nonapparent disability? According to the proposed bill, a nonapparent disability is a health condition that is not immediately obvious or visible, this could include developmental or intellectual disabilities. According to a study by the National Institutes of Health (NIH), [04] common nonapparent disabilities are anxiety and depression, Alzheimer's, deafness, post-traumatic stress disorder (PTSD), attention-deficit hyperactivity disorder/attention deficit disorder (ADHD/ADD), and diabetes among others. People with developmental disabilities are about seven times more likely to encounter law enforcement than neurotypical individuals, according to a 2001 study by the Department of Justice. [05] Citations: [WEBSITE] Legislation: Eric's ID Law , or HB707: https://tinyurl.com/4r5s8ntp [ARTICLE] Maryland mom and her autistic son pitch a disability safety bill on ABC’s ‘The View’: https://tinyurl.com/4nzukspm [ARTICLE] George Floyd's death sparks large protests, confrontations with police: https://tinyurl.com/263hk9sk [STUDY] Living with invisible medical disabilities: experiences and challenges of Chilean university students disclosed in medical consultations: https://tinyurl.com/bdexd9js [ABSTRACT] Contact with Individuals with Autism: Effective Resolutions: https://tinyurl.com/56d6yd44 [ORIGINAL ARTICLE] Proposed bill would allow Marylanders to disclose nonapparent disabilities on their IDs: https://tinyurl.com/9k7z6nyh
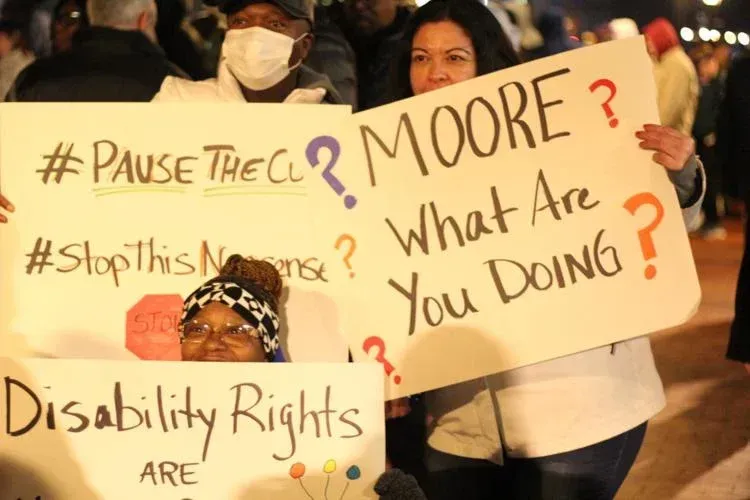
Advocates and service providers on the Eastern Shore are joining Maryland’s disability community to call for rollbacks on projected cuts to funding for developmental disability services. Scott Evans, executive director of the Benedictine School in Ridgely, said the near $200 million in cuts to Developmental Disabilities Administration funding outlined in Gov. Wes Moore’s proposed budget would be the worst he’s seen in his 25-year career. “Bottom line, these proposed cuts of close to $200 million in state funds would be catastrophic to the community service providers, as well as the people we support and our employees,” Evans said. “It would literally set us back years in funding.” The proposed cuts come as the state faces a near $3 billion deficit. Some advocates from the Eastern Shore note they could reduce the choices available for families and people with disabilities. Jonathon Rondeau, president and CEO of The Arc Central Chesapeake Region, says families and people with developmental disabilities on the Eastern Shore already have a limited number of options. “There are less agencies providing services for people with disabilities on the Shore,” Rondeau said. “So if there is instability in the system, it can potentially reduce choice for people with disabilities.” Evans echoed the same sentiment, and added that the cuts could hurt Benedictine’s ability to stay competitive when hiring employees. In recent years, the nonprofit school and service provider has raised wages in an attempt to attract quality employees. “All that has been an investment we’ve made because of the funding that we have received,” Evans said. “Now to wipe that funding out basically overnight means that we’re stuck in a holding pattern.” THE CUTS In Moore’s budget proposal, his office notes that in addition to the $1.3 billion set for the Developmental Disabilities Administration in fiscal year 2026, the state will “better leverage federal funding and align Maryland’s program more closely with federal guidance and practices across other states.” Evans says it’s not clear how DDA would implement the cuts, though his team at Benedictine team is working to crunch the numbers. Evans said it would cost the school hundreds of thousands of dollars of funding at the very least. Specific cuts that worry advocates include reductions in “dedicated hours” funding for those in community living programs, as well as a $14.5 million blow to self-directed services funding. “Someone who is in their late 60s and retired and chooses to stay home every day rather than going to a day program won’t necessarily have that choice anymore,” Rondeau said regarding the dedicated hours cuts. “There won’t be the funding available for that. It’ll be difficult for providers such as The Arc to support someone who may have significant health issues and need to go to the doctors.” Karenna Jones of Salisbury worries that cuts to self-directed services will impact the ability for her family to take care of her 26-year-old son, Kenneth, who has a traumatic brain injury and lives at home. Jones says as long as she lives, she “would never put (her) kid in a provider home.” But large cuts in funding may leave her with no choice. “We might be forced to do that,” Jones said. “It’s not fair.” RALLY IN ANNAPOLIS With the uncertainty swirling, hundreds packed Lawyers Mall in Annapolis Monday night, protesting for legislators to reject the proposed cuts. Leaders at the Benedictine School and The Arc Central Chesapeake Region attended, as did Jones. “I’m always amazed at how quickly the folks within the disability community can rally around a cause, and a cause that means so much to them,” Evans said. “And also, to some extent, the positive response we’ve gotten from legislators about these cuts.” Jones said the rally — organized with just three days notice by a developmental disability coalition — was inspiring and beautiful. “We were saying, ‘Save our DDA services. Save it. Don’t leave us behind,’” Jones said. Citations : [ORIGINAL ARTICLE] ‘Catastrophic:’ Eastern Shore advocates share impacts proposed disability cuts may bring: https://tinyurl.com/5ahffbu8